Understanding the cycle of pain and your mental health
Medically reviewed by Ms. Roisin Traynor, mental health counsellor
When living with endometriosis, pain is often a common, frequent symptom. Considered a chronic pain condition, it can have a persistent negative effect on your mental wellbeing. We’ve worked with our mental health counsellor, Ms. Roisin Traynor, to help explain the pain cycle of endometriosis and what she would recommend for coping strategies.
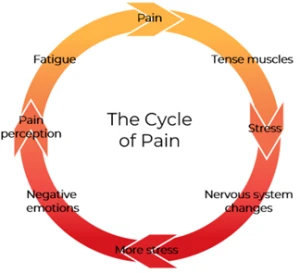
Roisin uses ‘’the cycle of pain’’, a bio-psycho-social model, to explain how living with a chronic pain condition can feel like one problem leading to another, which can make you feel trapped in a vicious cycle.
1. Feeling pain
Symptoms that cause pain will start the cycle. The NICE and ESHRE guidelines recognize symptoms like menstrual cramps, pelvic pain, painful sex, and pain when urinating or during bowel movements, but you may experience many other symptoms.
2. Tense muscles
As you feel pain, your body’s natural response is to tense your muscles. This is an automatic reaction as your body tries to protect itself from a perceived threat. If your muscles are tense (or contracted) for a long period of time, this causes reduced blood circulation and accumulation of lactic acid, which causes more pain in that muscle. This is common in patients with endo that have pelvic pain, pain when urinating, or painful sex, as the pelvic floor muscles over-contract and it is difficult to relax them.
3. Stress
Pain and stress go hand in hand. This stress triggers your nervous system to activate a fight-or-flight response because it thinks your body is in danger. Here, more physiological changes occur as your brain produces cortisol, adrenaline, and noradrenaline. You can experience heightened blood pressure, faster heart rate, increased inflammation, nausea, loss of appetite, and flare-ups of endo symptoms.
4. Negative mental health
It’s very natural to feel negative emotions when you are in pain: frustration, anger, fear, sadness, and helplessness are just some of the feelings that patients with chronic pain experience. Depression and anxiety are common in people with endo. These feelings can get worse if you feel like you are lacking support and understanding with what you are going through. This can be felt with intimate relationships and friendships, in the workplace, or when speaking with healthcare providers.
Unfortunately, this is counterproductive, since the negative emotions only create more stress. Constantly feeling negative can contribute to this vicious pain cycle and make it more difficult to effectively manage your pain.
5. Pain perception
It’s common to feel like you can’t stop thinking about the pain, and can’t focus on anything else. This is because as you constantly feel pain, your nerve endings keep getting excited and stimulated, which lowers the threshold for what is considered painful. This is called over-sensitization, which means that you might feel pain in situations that do not normally cause pain, like putting clothes on or something/someone touching you lightly.
6. Fatigue
Eventually, you get tired from dealing with the pain and emotions that accompany it, and become fatigued. Your body is trying to recover both mentally and physically. Unfortunately, sometimes the pain is so great that it can be difficult to rest. This puts you back into the vicious pain cycle.
How to break the cycle of pain and look after your mental health
Chronic pain can be extremely difficult to cope with and affect every area of your life. The most optimal treatment plan will be approaching your condition with understanding, education, and support. Every patient’s journey will be different. This can depend on what phase of diagnosis and treatment you are in, how much external support you’re receiving, and how your symptoms are affecting your quality of life. You should receive care that assists with both symptom and mental health management; after all, your mental health is just as important as your physical health.
Pain and stress are very intertwined; one can cause the other, making the spiral overwhelming and difficult to escape. It is possible to break free through coping mechanisms, but they take time to get accustomed to. By practising stress management, you can gain the ability to get out of the pain spiral. Helpful techniques and tools recommended by Roisin include:
- Self-Care including complementary techniques that help you relieve stress. Members of our endo panel have recommended gardening, acupuncture, reading, ASMR (Autonomous Sensory Meridian Response), slow walks, warm baths, exercise, or anything that helps them self-soothe.
- Journalling comes as a highly recommended strategy for mindfulness, especially for people with chronic pain.
- Guided breathwork / meditation using mobile apps can be a great way to learn how to focus on your breathing, and can be beneficial alongside light exercises like gentle yoga and stretches.
- Music, art and hobbiescan be used as a form of self-expression and creativity can move your mental focus away from your physician pain. Finding a state of flow!
- Mindfulness and pacing yourself can also be useful to help you be in the moment and transform the way you relate to and manage pain. A good method to help you connect to the present moment is the 5-Sense Meditation strategy. It involves using your 5 senses (seeing, hearing, feeling, smelling, and tasting), where you focus on them individually. This can help calm your nervous system by distracting you from focusing on the pain.
- Support groups are a great way to connect with other people who are going thorough similar experience. If you ever feel misunderstood, ignored, or unheard, it’s important to remember that you are not alone in this journey. Try to find online forums, local in-person support groups, or social media advocates that are sharing your experience. These communities can recommend specialists, coping techniques, and other helpful resources, or simply be a supportive presence for when you feel isolated.
Roisin recommends the following pages for support:
Instagram:
Online forums: Nancy’s Nook
Finally, Roisin recommends seeking help from a professional counsellor for further treatment. Therapies that can support life with chronic pain can include:
- Acceptance and commitment therapy (ACT) encourages you to accept your thoughts and feelings. You commit to actions to embrace the challenges you face and not avoid them.
- Compassion-focused therapy (CFT) helps you to respond to your own inner negativity with kindness and compassion.
- Cognitive behavioural therapy (CBT) helps you to change the way you think and what you do, by focusing on current problems and practical solutions.
- Integrative therapy draws on different types of therapies to make the counselling specific to your needs.
- Mindfulness-based stress reduction is the process of bringing your attention to the present moment. In this practice, you learn to simply observe all feelings, thoughts, and sensations you currently experience (both pleasant and unpleasant) and learn to accept them without suppressing or trying to control them.
If you need help now for yourself or for another person:
- Call a Helpline: Ring the Samaritans 24/7 on Freephone 116 123 (UK and Ireland) for immediate support for mental wellbeing.
- Text a Helpline: 50808 is a free 24/7 text service (Ireland). Text 3Ts to 50808 for immediate support for mental wellbeing.
- Call 999 or 112: In an event of an emergency.
- A&E: Visit your Accident & Emergency Department. Bring a companion, if you can.
- GP: Talk to your GP if you feel that your quality of life is being affected in any way by your symptoms.
Written by Joii Team